F.D.A. Approves a Drug That Can Delay Type 1 Diabetes
The Food and Drug Administration has approved the first treatment that can delay — possibly for years — the onset of Type 1 diabetes, a disease that often emerges in teenagers.
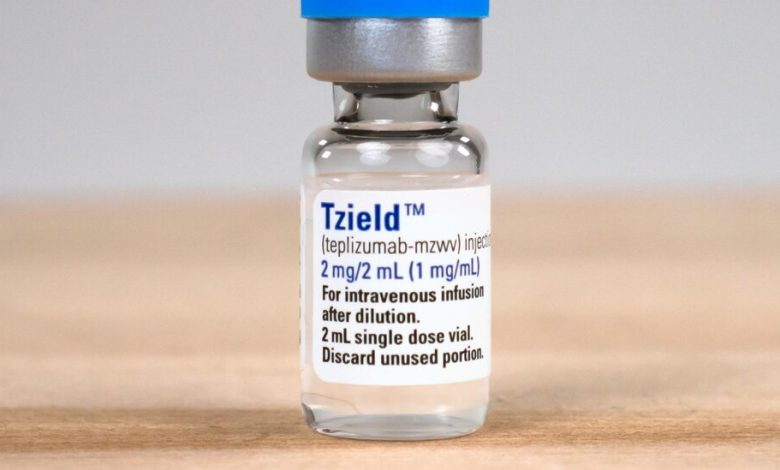
The new drug, tepilizumab, is made by Provention Bio, which will partner with Sanofi to market the drug in the United States under the brand name Tzield. In an investor call on Friday, Provention said the drug would cost $13,850 a vial or $193,900 for the 14-day treatment. The company said tepilizumab should be available by the end of the year.
The drug, which the F.D.A. approved on Thursday, does not cure or prevent Type 1 diabetes. Instead, it postpones its onset by an average of two years and, for some lucky patients, much longer — the longest so far is 11 years, said Dr. Kevan Herold of Yale, a principal investigator in trials of the drug.
The only other treatment for the disease — insulin — was discovered 100 years ago and does not affect the course of the disease. It just replaces what is missing.
Tepilizumab will be used to treat patients at high risk for Type 1 diabetes who have antibodies that indicate an immune attack on their pancreas and whose glucose tolerance is not normal. Treatment involves a 14-day infusion of the drug, a monoclonal antibody that blocks T cells, preventing them from attacking the insulin-producing cells of the pancreas.
“Talk to anyone who has Type 1 diabetes and any day you are not burdened by measuring blood sugar four times a day and injecting yourself with insulin is a glorious day,” said Dr. Mark S. Anderson, director of the diabetes center at the University of California, San Francisco, and a researcher for the pivotal clinical trial that led to the treatment’s approval. Dr. Anderson has been a paid consultant for Provention in the past.
Dr. John Buse, a diabetes expert at the University of North Carolina who was not involved in the study, called the approval “really exciting” and said it would “turn the world of Type 1 diabetes on its head.”
“There has always been a notion that screening would be a good idea,” he said. But medical experts “have never really promoted it to detect Type 1 diabetes.”
It will not be easy — no screening test is. But in this case, very few who are screened will have this rare but dire disease, which affects just four in 1,000 in the general population, or 1.4 million Americans.
Type 1 diabetes typically emerges in adolescence when patients suddenly are tired all the time, urinating frequently, drinking copious amounts of water, and losing weight.
With a diabetes diagnosis, their lives are completely changed. They have to measure their blood sugar and take insulin for the rest of their lives. Every time they eat a meal, they have to calculate how much insulin they need. If they take too much, they can pass out or have a seizure or even end up in intensive care.
They also face the specter of complications — eye disease that can lead to blindness, kidney failure, heart disease and stroke. Without good control of blood glucose, complications can set in as early as five years after diagnosis, Dr. Anderson said.
The new treatment, Dr. Anderson said, “opens the door,” much in the way that the first immunotherapy for cancer was a breakthrough to a new era of treatment about a decade ago. He expects that as immunotherapy for diabetes improves, the disease may be halted before it can take hold.
The new drug is not a treatment for the much more common type of diabetes, Type 2, in which the pancreas makes insulin but the body’s cells do not respond to it.
The story of the new treatment dates back to the 1980s and involves determined researchers who pursued the idea as company after company — four in total before Provention — got interested but then ended up dropping the drug for a variety of reasons.
Dr. Jeffrey A. Bluestone, an academic until recently who is now chief executive of Sonoma Biotherapeutics, said he and his colleague, Dr. Herold, who has consulted for Provention and other companies, spent 20 years “trying to keep the drug alive.”
“Scientists were passionate about it,” Dr. Bluestone said. “Guys at companies were really passionate about it.” But for reasons unrelated to its potential, it kept being dropped.
Dr. Herold said he vividly remembered trips that he and Dr. Bluestone and a French researcher, Lucienne Chatenoud of Paris Descartes University, made to drug companies “begging them to pick this thing up.”
At one point, Dr. Bluestone actually took the antibody, developed at that time by Ortho Pharmaceuticals, and made a clinical batch of the drug in the lab. Dr. Herold tested it in a small study of people who were newly diagnosed with Type 1 diabetes.
The treatment prolonged the period in which they made some insulin, but eventually all got diabetes.
In 2011, Dr. Bluestone and Dr. Herold proposed a different sort of study. They would treat people who were at high risk of diabetes but who had not yet developed it. It was a bold move, Dr. Bluestone noted. “Other than vaccines, there aren’t many drugs given before diagnosis,” he said.
To find those people, the researchers worked with a group of clinical trial sites, TrialNet, that were supported by the National Institutes of Health. Dr. Herold is now the group’s chairman. TrialNet investigators screened 200,000 people who were immediate family members of people with Type 1 diabetes, looking for antibodies indicating an immune attack on the pancreas and abnormal glucose metabolism.
The result was a study, published in the New England Journal of Medicine, that led to Thursday’s approval.
Now that the drug is approved, the challenge will be to find people who could benefit. Screening only people with immediate relatives who have diabetes will miss 85 percent of patients.
The JDRF, a nonprofit group that advocates for people with Type 1 diabetes and supports research, which, along with the N.I.H., funded the trial that led to the drug’s approval, wants antibody screening tests to become part of routine pediatric care.
“Most families say diagnosis is a bolt out of the blue,” said Aaron Kowalski, chief executive of the JDRF. And most patients, he added, are very sick when they first are diagnosed.
The group has conducted blood tests to look for antibodies in Germany and in parts of Colorado. And it has offered an at-home test people can order, underwritten by the foundation. But, Dr. Kowalski said, “we want pediatric offices to do it.”
Testing also offers another opportunity, he said. It turns out that antibodies indicating an immune attack often occur when people are as young as 5 or 6 years old, although most do not develop diabetes until they are teenagers.
Now, he said, his hope is to treat people even earlier, as soon as those antibodies emerge. Clinicians and the F.D.A. had previously objected to treating before the disease was clearly underway, asking, “How can you give an immunotherapy if they are normal?” Dr. Kowalski said.
But, he said, the antibodies tell a different story.
“They do have diabetes,” he said, although not according to the usual definition of the disease. “It just hasn’t unmasked itself yet. We need to help them save their beta cells,” the insulin-secreting cells of the pancreas.
Dr. Herold is cautious. If someone has antibodies but their pancreas is not actively being attacked, the treatment may not help.
“It’s hard to stop something that isn’t happening,” he said.
Dr. Bluestone and Dr. Herold wonder if giving a second round of treatment could improve results even further.
For now, Dr. Bluestone would like to see the treatment used to help younger patients than were in the trial. It is approved for patients at least 8 years old. “But the disease affects a lot of patients who are younger than 8,” he said.
Although he and others are excited about the possibility of some day preventing the disease entirely, there is an immediate challenge for diabetes experts.
“The most important thing right now is finding the potential patients,” Dr. Bluestone said.
