Maximizing Profits at the Patients’ Expense
More from our inbox:
- The Brave Trump Jurors
- Black Voters ‘Want to Be Courted’ by Democrats
- Better Than Debates

Credit…NA
To the Editor:
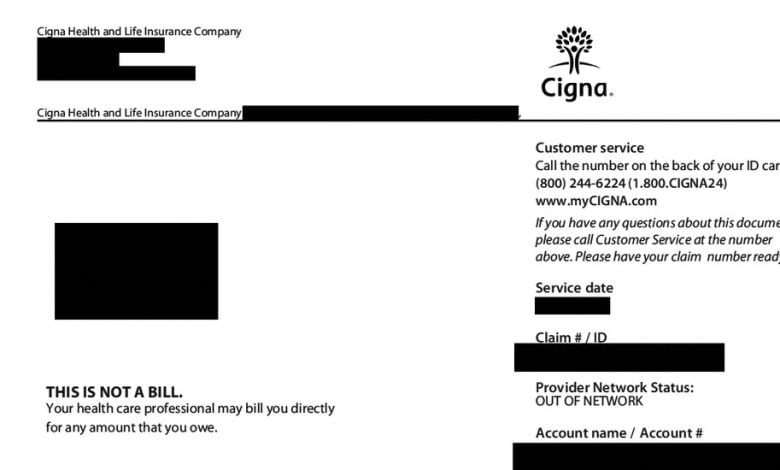
Re “Patients Hit With Big Bills While Insurers Reap Fees” (front page, April 7):
Chris Hamby’s investigation uncovers the hard truth for patients who receive care from providers outside their insurance network. While most of us try to save out-of-pocket costs by using in-network health professionals and hospitals, it’s not always possible. And there’s no way to determine what we’ll owe until after we get that care — when it’s too late to reconsider based on the costs we’ve incurred.
So, it’s more important than ever for the government to swiftly implement an essential element of the No Surprises Act: Providers should have to give patients an advance explanation of benefits so patients can estimate their financial burden before they get treatment, in or out of network.
Health price transparency is improving, but it’s outrageous that even two years after the No Surprises Act passed, everyone except the patient knows the price of a procedure or doctor’s visit in advance, leaving patients unpleasantly surprised.
Patricia Kelmar
Alexandria, Va.
The writer is senior director of Health Care Campaigns for U.S. PIRG.
To the Editor:
This is just the latest example of the schemes deployed by insurers to maximize profits by cutting reimbursements to physicians and shifting medically necessary health care costs onto patients.
Whether it’s through third-party entities like MultiPlan or using tactics such as narrowing provider networks and restrictive prior authorization policies, insurers have the perverse incentive to boost revenue over offering adequate payment for quality patient care under the guise of “controlling costs.”
More and more patients are being forced to decide whether they should forgo treatment because their insurer won’t pay the bill.
